The world of health care is complex, for both you and your employees. Get the right support to the right people at the right time, based on their needs, health risks, and medical conditions. HealthCheck360 offers a full suite of personalized care options spanning the diverse health needs of your population.
HealthCheck360's Advocacy program puts healthcare and benefits experts within reach, connecting your employees to the support they need when they need it, saving them, and your plan, valuable time and money. With an ROI of 250%, results are the norm.

We take a different approach to condition management. Focusing on four unique strategies, we create a personalized experience that helps members stay compliant with their recommended care and improve their health, all while reducing costs for your health plan. Clients have saved over $2,000 per member each year.
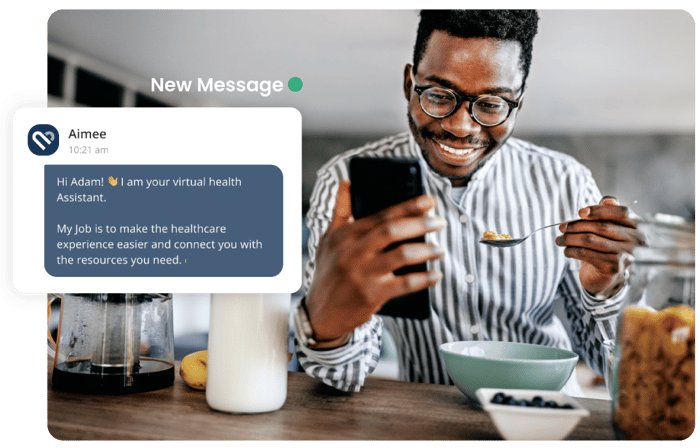
The myHealthCheck360 platform connects your employees with resources to support their well-being, anytime, anywhere. Our mobile app, participant portal, automated trackers, and daily rewards make it easy for your users to take control of their health.

Utilization Management (UM) is the evaluation of medical necessity, appropriateness, and efficiency of the use of healthcare services, procedures, and facilities under the auspices of the employee benefit plan. Utilization Management encompasses prospective, concurrent, and retrospective review in which evidence-based, clinical criteria are applied to a request.

“THANKS TO MY HEALTHCHECK360 NURSE, I NOW HAVE
THE DIRECTION I NEED TO TAKE BACK MY LIFE AFTER YEARS
OF LETTING MY CONDITION CONTROL ME."
HEALTHCHECK360 PARTICIPANT
LEARN MORE ABOUT INTEGRATED CARE MANAGEMENT
Request more information to learn how we can customize a program that fits your needs.