TABLE OF CONTENTS
01 Chronic Care Management vs. Health Coaching | 02 Supported Conditions | 03 Employer Needs | 04 Goals of Chronic Care Management | 05 Incentivizing Chronic Care Management | 06 Member Identification | 07 Outreach Methods | 08 Results | 09 Supporting Those Without Chronic Conditions | 10 Population Health Strategy | 11 Additional Resources
![]()
Chronic Care Management programs can go by many names. Disease management, condition management, and medical management are all terms commonly used. Regardless of what you call it, these patient-focused, high-touch interventions helps individuals manage chronic conditions, which in turn drives down costs and improves compliance with their physician’s care plan.
In the United States, the national prevalence for diabetes is 9.3% overall and 1 in 3 U.S. adults have high blood pressure. These people are driving up to 80% of the medical spend and cost a company's plan 2.2 times more than members without a chronic condition.
It doesn't have to be this way. Supporting these people in managing their condition in turn controls costs, while improving health.
![]()
One of the big differences between chronic care management and health coaching is the clinical nature of the program. Chronic condition management is generally provided by a nurse, whereas health coaching is provided by someone with a health, but not necessarily clinical, background.
According to Employee Benefit News, “A good condition management program includes guidance on nutrition, exercise, sleep and stress management, but how those areas are prioritized should depend on the individual.” For example, if a participant’s poor nutrition habits are a result of their stress levels, tackling their stress and offering stress management tools is prioritized first.
The last key difference between coaching and chronic care management is that chronic care programs are offered only to members who have certain chronic conditions. Health coaching is generally available to all members or those who have one or more significant health risks, but haven’t developed a diagnosed condition.
Employers want to help keep their employees healthy and control costs. Supporting people with serious medical conditions like diabetes and high blood pressure delivers employee longevity and vitality while reducing some of the most costly claims on their health plan.
IMPROVING HEALTH TO MANAGE COSTS
Many employers understand that a company wellness program is essential. According to Mercer’s National Survey of Employer-Sponsored Health Plans, 80% of employers with 500 or more employees listed managing high-cost claimants as their top health care priority in the next five years. To reduce health plan costs, employers must focus on supporting their highest-risk and highest-cost employees. When these individuals receive the care they need, employers save around $2,000 per member each year.
To provide this population with daily personalized care, companies are looking for tech solutions:
• 56% of employers are prioritizing health technology solutions
• 68% want apps for managing conditions or reducing health risks
• 2 in 5 employers have the budget to spend on new tech
TECHNOLOGY TAKES THE GUESSWORK OUT OF MANAGING A CHRONIC CONDITION
Technology offers accessibility, meeting your employees at a time and place that’s always convenient for them. With HealthCheck360’s myCare360 app, users get reminders about upcoming appointments, labs that are due, and medication compliance, all personalized to the user.
04/
![]()
Motivating your employees to improve their health should be the top priority of your condition management program. As you evaluate a program, keep these 5 goals in mind:
![]()
SUPPORT
Encouraging the relationship between the member’s physician and their plan of care.
![]()
RESULTS
Monitoring claims and health data to ensure the program effectively lowers your health plan spend.
![]()
PREVENTION
Reducing the risk of future medical complications related to the condition using evidence-based care guidelines.
05/
![]()
Deciding to incentivize your chronic care management program has a lot to do with your company’s goals. If you’re seeing skyrocketing health care costs due to hospital admissions or emergency care related to chronic conditions, it might be worthwhile to provide members with incentives for participating in a chronic care management program or complying with recommended care. If you’re looking to enhance your benefits, just having a chronic care management program and advocate available to the members can be incentive enough.
Rewards and incentives can vary, but the most common incentives we see include:
- Plan premium discounts
- Free or reduced cost medical supplies
- HSA contributions
- Gift cards
06/
![]()
Many times members are offered a condition management program as a voluntary benefit. At HealthCheck360, we proactively identify members though medical and pharmacy claims, biometric screenings, health risk assessment surveys and referrals from other programs like utilization review. From there, we enroll all members with a chronic condition resulting in a 100% enrollment rate.
When evaluating a chronic care management program, make sure you’re informed and aware of the process for enrollment. You want to be sure you’re not missing eligible members. Unmanaged conditions can cost more than $2,000 per patient in avoidable treatment each year.

07/
![]()
Most chronic care management programs are telephonic. This allows your members to connect with a clinical expert at a time and place that is convenient and confidential for them.
Outreaches are good, but we believe in creating a two-way conversation with our members. We use technology to help get in touch with members. A continual flow of data from biometric devices also allows our nurses to support participants when they need it.
08/

Most condition management programs focus on checking boxes. If members receive a letter or call to discuss their health, they're marked as compliant even if they aren't actively managing their condition. While communication is important, we know that you need true engagement and cost results.
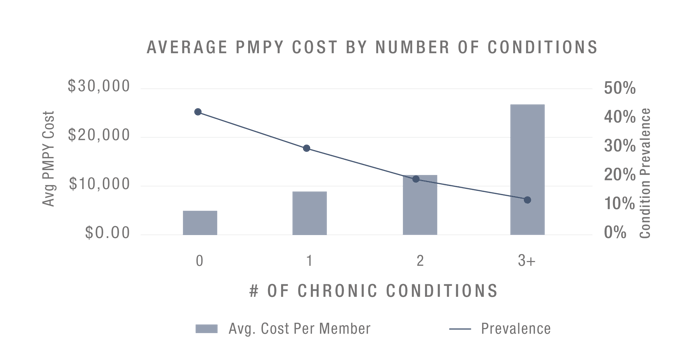
The national average for condition management compliance rates hovers around 30% – 40%. This should be the minimum benchmark for your company in determining if your program is successful. Each employee with an unmanaged chronic condition has a huge impact on your health plan spend, and when employees are diagnosed with more than one chronic condition, your per member per year (PMPY) costs skyrocket.
At HealthCheck360, we obsess over results. Through our unique program and flexible rewards solutions, our clients see compliance rates around 75% – 95%. With more employees engaged in managing their conditions, your health plan costs decrease. Our clients save over $2,000 per targeted member each year.
09/
![]()
Providing support for members with chronic conditions is incredibly important and successful at moving the needle on health and claims costs. But what about clinical support and care recommendations for employees without chronic conditions? We all know that prevention is important and helping people understand what preventative exams they need at certain points in their life is key to managing long-term health.
Supporting employees without chronic conditions can take many forms from education and support about preventative visits, to specific coaching programs like weight management or nicotine cessation, to general lifestyle coaching for healthy habits. We recommend supporting your employees without chronic conditions with health coaching.
Learn more about Health Coaching.
10/
Determining if a chronic care management program fits into your company's overall population health strategy is no small task.
Here are a few questions to consider when starting this process:
1. WHAT ARE YOUR GOALS?
2. WHAT IS YOUR BUDGET?
3. WHAT IS YOUR COMPANY CULTURE?
4. WHAT DO YOU NEED IN A PARTNER?
Learn more about why these questions are important and get help determining your population health strategy with this free checklist!