On-Demand Webinar | Running for Your Heart
February is Heart Health Month—a perfect time to focus on the habits that keep your heart strong.
1 min read
 HealthCheck360
:
Feb 13, 2020 11:15:00 AM
HealthCheck360
:
Feb 13, 2020 11:15:00 AM

The answer to higher healthcare spending isn't just about raising deductibles. This complicated issue involves looking at different solutions and investigating what is causing a rise in claims. Read on for a few strategies.
A recent study found 84% of healthcare spending can be attributed to just 20% of users. Many of these users have multiple chronic conditions, like diabetes and hypertension, and are are trying to manage primary physician visits, costs of prescriptions, and labs. But just raising deductibles, like 39% of businesses surveyed planned to do, doesn't address these people who are consistently reaching their deductible every year and need help managing their care.
That's where programs like Condition Management come in. By closing gaps in care, you can proactively help these users manage their health and reduce costs for both you and the employee. Our team of trained medical staff delivers a personalized experience for each member, while our data-driven technology makes it easier for the user to manage their condition.

February is Heart Health Month—a perfect time to focus on the habits that keep your heart strong.
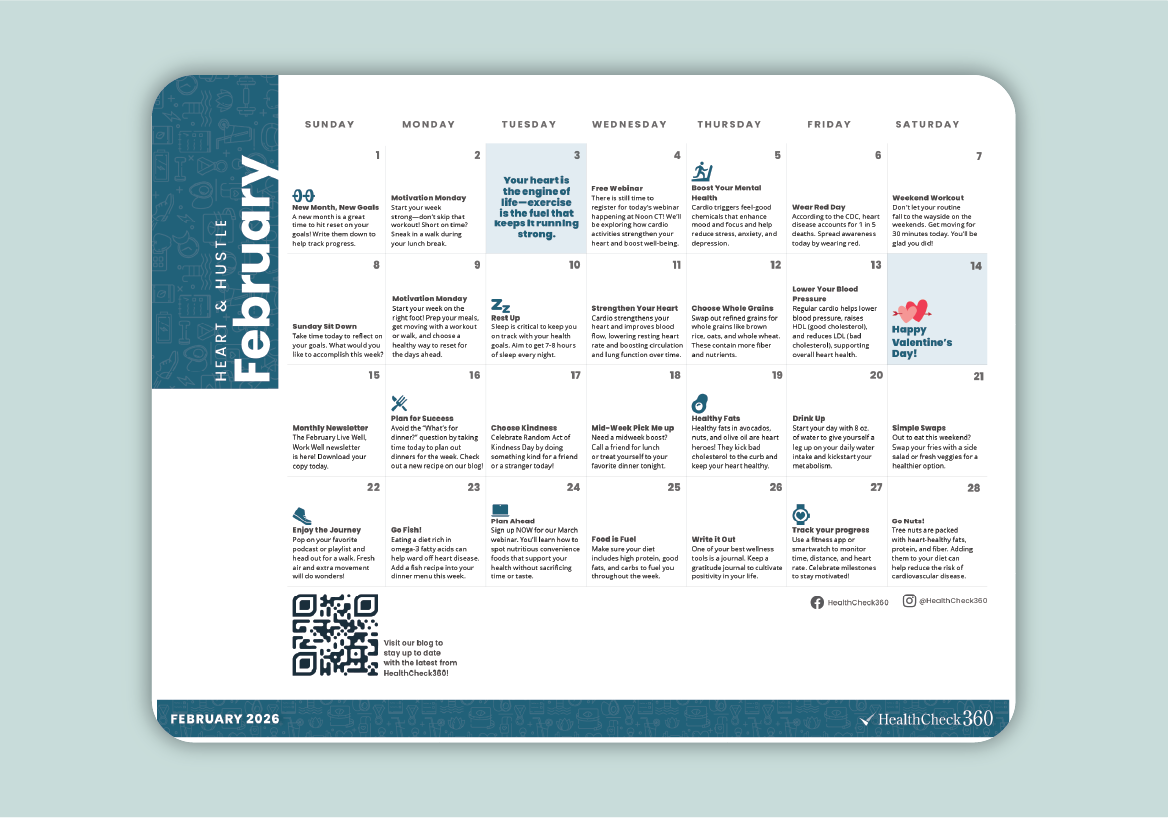
February is the perfect time to inspire your team to focus on their health and build habits that last. Our February Well-Being Calendar is a simple,...

Empower your employees to find their “why” and drive lasting change with our January on-demand webinar!