On-Demand Webinar | Running for Your Heart
February is Heart Health Month—a perfect time to focus on the habits that keep your heart strong.
2 min read
Jenna Wesenberg
:
Feb 11, 2019 1:19:00 PM

Did you know that condition management, or chronic care management programs go beyond keeping patients compliant with care? Condition Management helps close the knowledge gap for members. From helping patients understand their condition, what it means to their long-term health, helping them understand their medical bills, to learning about what each prescription does, condition management goes way beyond checking the boxes.
Studies show that between 33% and 50% of employees don't understand their benefits. This leads to poor utilization and unfortunately, the COVID-19 pandemic only widened the knowledge gap among American health plan members. Over 40% of US adults have a chronic health condition and those people are employees at your company. Without a condition management program, these employees are left to navigate the healthcare industry and their condition alone.
HealthCheck360 data shows that 59% of adult members who incur medical claims had at least
one chronic condition like diabetes or hypertension. Condition Management programs are one way to help close the knowledge gap among your members and control health care costs for your plan.
Here are just a few of the ways chronic care management programs educate your members and save your plan money:
Is your condition management program working for you? Learn everything you need to know about condition management and chronic care management programs here.
You can also contact us for more information or check out the webinar recording below for ways to keep your highest-cost employees getting the right care.

February is Heart Health Month—a perfect time to focus on the habits that keep your heart strong.
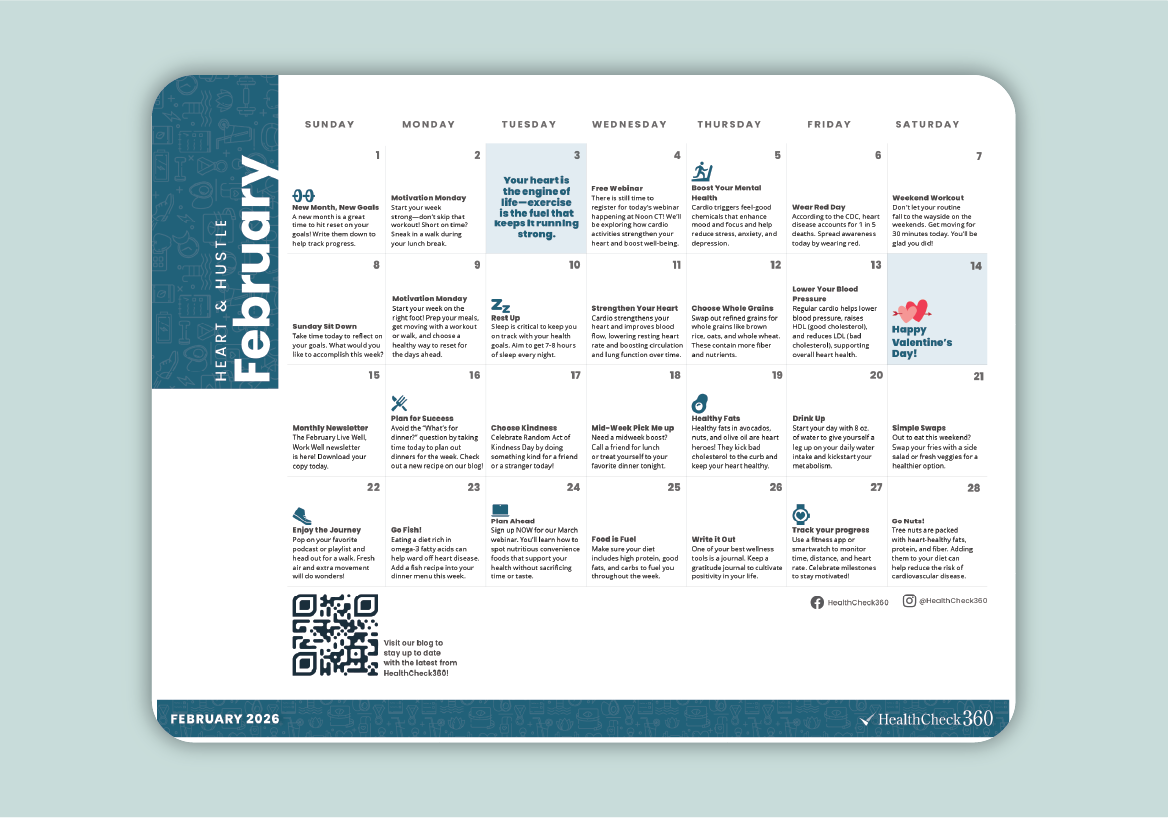
February is the perfect time to inspire your team to focus on their health and build habits that last. Our February Well-Being Calendar is a simple,...

Empower your employees to find their “why” and drive lasting change with our January on-demand webinar!